AH089 - Some [Healthcare] Data Visualization Treats, with Andrew Tsang
![AH089 - Some [Healthcare] Data Visualization Treats, with Andrew Tsang](https://cdn.prod.website-files.com/689e01a0fcf0d0ea17cb9b89/6903e81c58c51b4178f8f1d4_2025-10-30_Podcast_089_Graphics_Article%20Main.png)
On Episode 89 of Astonishing Healthcare, we are talking about some "visual treats," as the title suggests! Our guest, Andrew Tsang, has been posting some very cool things on LinkedIn of late, including Sankey and other dynamic charts highlighting where the money flows in healthcare (from the premium dollars to the care plan members receive), and which stakeholders win or lose in different scenarios via a 5-Way Seesaw he developed using AI! If you're a [healthcare] data nerd, this episode is definitely for you, and you'll want to check out:
- How many layers are between your employer's healthcare dollars and care? on LinkedIn (you can see where every $100 an employer spends goes!)
- What would happen if power actually shifted in healthcare? on LinkedIn (5-Way Seesaw)
Andrew discussed how and why:
- A significant portion of the healthcare premium is consumed by administrative layers and middlemen before ever funding patient care.
- Employers can combat wasteful spending by demanding full access to their claims data, then identifying and eliminating things that extract value from their plans (or don't work for their populations).
- Integrated care models (like Kaiser Permanente) and direct primary care help eliminate friction by aligning provider and payer incentives, allowing doctors to focus on practicing medicine (vs. revenue cycle management).
- New technologies like AI-powered prior authorizations may reduce administrative costs for payers but risk creating new burdens for providers and patients, if we're not careful.
- Hospitals face a fundamental conflict: core, life-saving services like ICU and emergency care are often unprofitable and must be cross-subsidized by higher-margin procedures.
Listen in below or on Apple, Spotify, or YouTube Music!
Transcript
Lightly edited for clarity.
Justin Venneri: (00:22) Hello and thank you for joining us for another episode of the Astonishing Healthcare Podcast. This is Justin Venneri, your host and senior director of communications at Judi Health. And I think we've got an audio treat accompanied by some visual treats in the show notes for you today.
Andrew Tseng is with me in the studio. His LinkedIn posts caught my eye recently, and so I figured we should have him on the show to explain some stuff that we talk about all the time. That includes where the money goes for care in this country and winners and losers. Andrew, thanks for joining us today.
Andrew Tsang: (00:50) Thanks so much, Justin. It's quite an honor to be here. I'm going to be honest, I'm really excited about this opportunity to talk a little bit more about what I've been sharing.
Justin Venneri: (01:02) I was very excited when you responded to my LinkedIn message. So it's always nice to know that people read stuff.
Andrew Tsang: Well, it was good. It wasn't just the, “Hey, I saw your interesting background, like, send me your resume please.” It was like pretty cool. You sent me fun emojis. (🔥 ones, actually). So I was into that.
Justin Venneri: So tell us a bit about your background and what you do for a living and then we'll get to what caught my eye online and some of the data and observations that I think everybody's gonna love.
Andrew Tsang: (01:20) Yeah. So Andrew Tseng, management consultant and technology consultant. I've worked for about 15 years across hospitals, health systems, insurance and health plan. Even done a little bit of pharma work like manufacturing, gowned up and got into the lab there.
Most recently started to touch a little bit of policy, which has kind of given me, I think, a really good breadth across the spectrum of healthcare. It's given me, from my perspective, this really neutral observer status. Feel like I'm kind of like Switzerland a little bit. And I don't really take any sides to it, but I see kind of like across the board what the dysfunction is and wanted to share my thoughts on that.
Justin Venneri: (01:51) Yeah, and I think you started a Substack too recently, Health is Other People?
Andrew Tsang: (01:55) Yeah, I'm particularly proud of that. It's just a place for me, I feel, to start sharing my observations and perspectives. Wanted to put out some objective analysis as well as my subjective experience. I think there's a lot of room in healthcare to create entertaining and informative content that really helps people untangle this really complicated mess we've got.
Justin Venneri: (02:16) Agreed. And you know, unfortunately we hear and see that a lot these days. It's messy out there. Part of the reason we're here is the system tends to reward companies that can take advantage of opacity [and/or] healthcare consumers ignorance and some of that messiness. So your post on the layers of spending, I shared that with my team instantly. That visual is amazing. We'll put that in the show notes along with a link to your Substack. I think we have a new one for you that you're working on right now. So maybe just focusing on that first one. How did you come up with that concept and that sort of flowchart of where the, you know, if you spend a hundred dollars, how does that go toward the members care? And then I have a few follow up questions for you, but start there.
Andrew Tsang: (02:52) Yeah, for sure. Well, I'll start by saying the flow of money in healthcare is just so complicated. I found a lot of success on LinkedIn honestly, and I'm at heart a data and visualizations guy. I really like these like Sankey diagrams that they call the show the flow of things across different stages. Some of them have done really successfully in my neck of the woods.
But anyways, so I keep seeing questions on, “Hey, where does our money go? Like, what happens there?” And there’s not really a good answer. So I built that flowchart specifically thinking about commercial plans and what's involved in insurance and administering commercial claims. So I built that flowchart of looking at things like, you know, your employee contribution plus your employer contribution and where does that actually go? So that flowchart started tracking every dollar from premiums all the way down through the administrative layers to actual care. And you know, spoiler alert, I'm sure everybody knows a lot of it disappears into these like intermediary layers before a doctor even sees a patient.
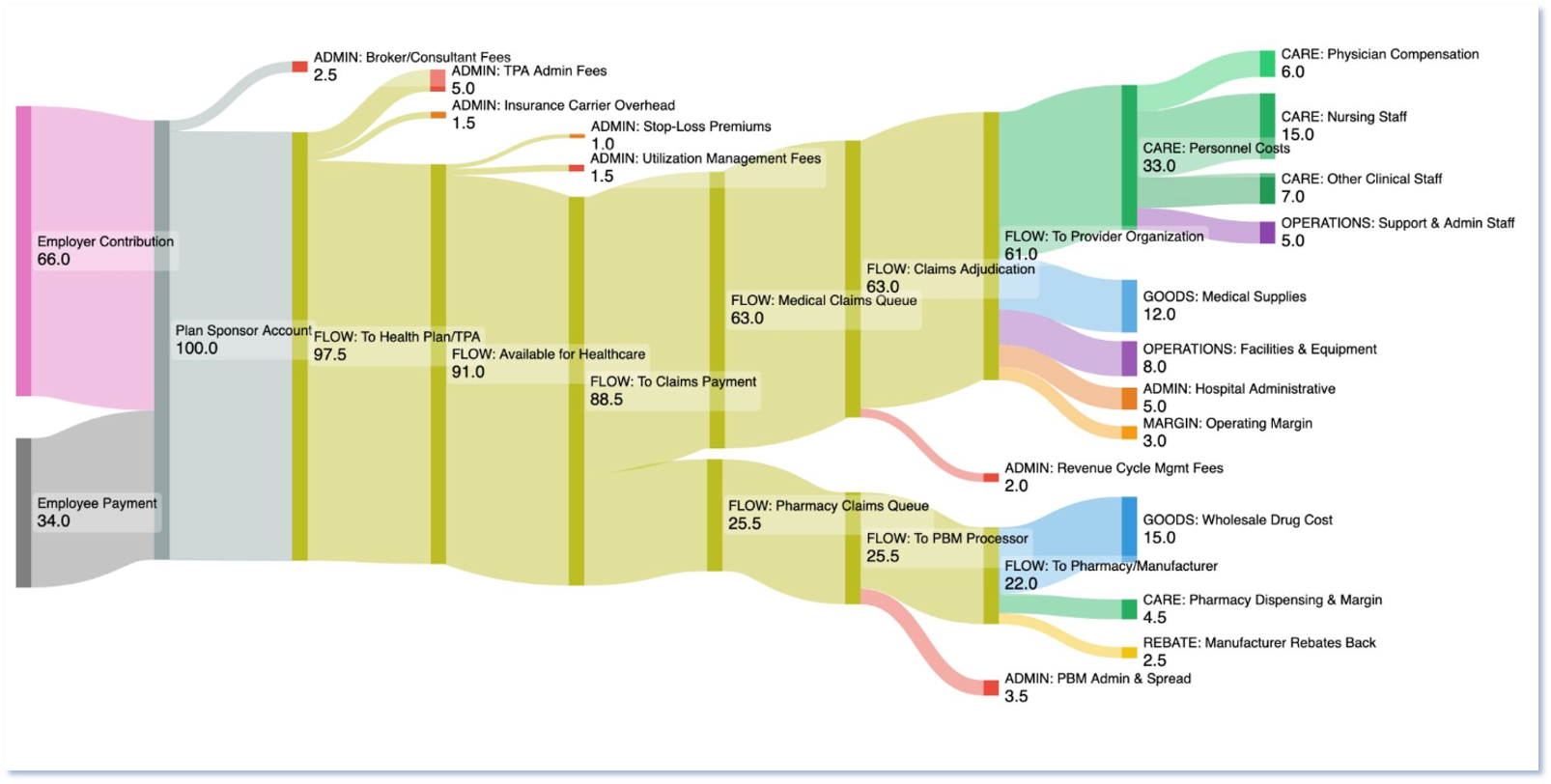
Justin Venneri: (03:50) And are they tolls, middlemen? Can you talk us through a couple of things extracting those dollars from the plan or from the care?
Andrew Tsang: (03:57) Well, definitely. In economics, you know, we think about things as value creation, value extraction. And it's always tricky. When I say extraction it feels bad, but you know, having been with a lot of administrators, I get it. But quite frankly, are these like middlemen, right? Are these tolls? I think some of it is like uber, right where it actually connects you to where you need to go. So there is value in that. It's funny, when the Internet first came out, people were like, oh yeah, this will be the death of all middlemen. But instead they've proliferated even more. Right. You've got Airbnb. You don't book a room directly, right. You don't get a ride from a taxi direct, you go through Uber. So there's some of that too.
But then there's things for sure where there's like a lot of toll booths as well, prior authorizations that don't actually improve outcomes. Verifying this information, that's not super important, it's just administrative burden. That's definitely like a toll booth in a middleman that kind of extracts value as opposed to some of the insurance stuff, which is like risk pooling and you know, there's some value to that.
Justin Venneri: (04:48) Did you take a look at what the major sources of potential waste in that spending breakdown or the friction you did break down where every dollar goes, which is great. We always tell plan sponsors to get their data, get their actual contracts, review and analyze everything and use that info. So where do you think plan sponsors could look for savings in your opinion?
Andrew Tsang: (05:08) Oh, gosh. I mean, it's tricky, right? For one, there's a couple of things you want to look at places that do more transparent pricing. I think reference-based pricing is very good because then you're able to see what things cost. There's a lot of opacity in the flow of the dollar. So, I know some companies, they do like spread pricing where it's just a fixed rate, so they extract some value out of there.
Health Benefits Data & Other Related Content
- How to obtain Rx data and what to do with it
- AH030 - Plan Sponsors Need a Source of Truth; Get Your Data Now & Find It, with Jeff Hogan
- Capital Rx Unveils Healthcare’s First Unified Pharmacy and Medical Claims Processing Platform
- Pharmacy Benefits 101: Prior Authorizations
- AH048 - High-Cost Orphan Drugs, Securing Claims Data, and More, with Dr. Eric Bricker
Justin Venneri: (05:28) Very familiar with that here in the PBM, not us, but see a lot of spread there.
Andrew Tsang: (05:32) Yeah, I think that's been a common theme. And you're right. In Judi Health, you guys aren't doing that, which is good because I think that's a big part of it, right? Where then you're losing a lot of... where does the value actually go? So I pulled the data from like CMS's National Health Expenditure data. This is like government reported data, right? There's like an annual report and you can see where money goes in there. To be honest, it is hard, right? You know, we've been trying to beat the drum of reducing healthcare costs in this country for a long time and there's a lot of trade offs there and it's hard to really figure it out.
But for one: administration. I think people can wholeheartedly agree that if there's a lot of admin that is just creating more burden from your premium dollars to patient's care, definitely not worth it. So, I think employers can definitely think about ways through there, seeing really interesting trends through like price transparency or like direct contracting that are interesting ways that potentially people can save a lot more on what they spend.
Justin Venneri: (06:21) You mean for specific services like infusion or other direct contracting with providers? Direct primary care has been around for a while and it seems to be there's more direct primary care places popping up. Is that kind of what you're referring to?
Andrew Tsang: (06:33) Yeah, I think some interesting models through there. I think right now, as employers need to manage their benefits and their annual spend on that, they're going to need to think about creative ways to provide the services to their employees that are really going to be most valuable and whether that's going to be, you know, cohort specific services or they're going to have specific, you know, new models of care.
I've heard people, you're a large enough employer, just talk to your local health system, right? See if you can negotiate like a contract that way. I'm sure people have been exploring those options too, but it's hard. There's a lot of stickiness and momentum that needs to be created before we can go down that route.
Justin Venneri: (07:07) Do you think there's anything that could help reduce the layers? I think when people see the chart, if they haven't seen the chart already, but wow, there's a lot of places where dollars are siphoned off or allocated to wasteful things or to useful things between the premium dollar and the actual care that they're receiving. So I'm not going to get up on a soapbox and yell about unified claims, but it's interesting to see how many stops there are for money. Do you see the potential for something like unified Claims to help?
Andrew Tsang: (07:30) [laughter] Maybe [you’re] leading the witness here, but...
Justin Venneri: Definitely…
Andrew Tsang: Unified claims could definitely help. I think what was interesting about the visualization, and you guys should check it out, if you're just listening to this, you can see like the split and you see that medical, dental, vision, pharmacy, they all speak different languages and that creates a lot of translation overhead. But honestly, here's the catch though. Every layer can point to like the value of what they add. Right. And you know, some of it is real. But, you know, cutting layers, you know, means changing the incentives. And it's way harder than just saying, okay, we need less admin and bureaucracy. There is some tough decisions we need to make collectively in this healthcare system.
Justin Venneri: (08:05) And we often say to follow a dollar and sorry for leading the witness on that last Question. I try not to do that with the path you've laid out. And I agree there's value embedded in some of those flows, for sure. The idea is to see who profits from what and what the return is if there's an ROI. How do you think employers, for example, could sniff out that wasteful spending if everyone justifies their spend in different ways?
Andrew Tsang: (08:27) Well, I'll say this for now. One, the first thing is the employer is getting their data. I think that's what you're alluding to as well. I think that's super important is that if an employer is spending all this money, they should know what they're getting out of it. And sometimes there's the ERISA laws with the fiduciary responsibilities need to be able to see what they're spending and adequately assess what they're spending is getting the right value. And it is going to be different depending on your employee groups, you know, so different families have different needs and things like that. So it's really incumbent and it's a lot of burden. Right. Someone who's like a benefits administrator is going to need to learn a lot about healthcare if they aren't already.
And I think that's a big part of sniffing out what things won't be as valuable. Right. Seeing, okay, are they getting the most spend there? Maybe looking at things like high-cost claimants, looking at areas where we're seeing there are high amounts of spend that they could probably better manage, maybe, I don't know, through things like steerage or some kind of benefit design. And employers hold the most leverage because they're the ones signing the checks. They should think about how they're spending that money and ultimately reduce healthcare costs in the U.S.
Justin Venneri: (09:30) I think it's a good point that they do have a lot more leverage and I think they know that. But I think sometimes they're just busy. They have a lot of other stuff to worry about aside from health benefits too.
Andrew Tsang: (09:37) Yeah.
Justin Venneri: (09:38) So you've worked with providers, systems, payers across the country. Curious if you see anyone doing things particularly well that you'd like to highlight or if you want to highlight the things you're seeing that make sense or are working with or without names.
Andrew Tsang: (09:50) It's totally fine for one. And this goes back to my ethos of that, you know, healthcare when it first developed, it was all very like siloed, like things kind of just converged into the system that we call us healthcare. So it's really important to see systems that are really thinking more holistically, maybe with a lot more breadth across populations or across the stack in terms of delivering care and the healthcare finance of it.
Seeing a lot of different places and you know, I'll just name names Kaiser Permanente, I think they do a lot where its physician led, it's integrated because you're having provider and payer incentives under one roof. So, you eliminate a lot of that friction that we're talking about through all the different layers. I'm also seeing different models too, like direct primary care, which we kind of mentioned a little bit earlier. I think it's a great model because it's removing things like billing complexity across primary care. And that's appealing, right? So, doctors can actually practice medicine instead of just, you know, managing this whole idea of revenue cycle.
Justin Venneri: (10:45) Makes sense. Your Substack and another LinkedIn post of yours. Talk to me a little bit about this 5-way framework or “Seesaw” that you've created. I think this is one of the treats we're sharing today.
- See What would happen if power actually shifted in healthcare? on LinkedIn for more.
Andrew Tsang: (10:55) One of the things that I've done across my career has been across different stakeholders, so provider, payer, pharma and so forth. And one thing I thought was funny is just breaking out the different stakeholders that way and thinking about, okay, who benefits or who has different incentives in these models. One thing I ended up doing was creating a little app called the Healthcare 5-Way Seesaw. I've always thought about it as a cheeky little thing. Everybody knows what a seesaw is, but like a five-way seesaw, you're like, okay, what does that mean? Like how do things shift up and down? Right. So I thought it was like a sticky idea and it was cool.
Andrew Tsang: (11:26) Some folks reached out to me, policy folks or different people who do research and they were like, this is like a really fun way to think about it. So from this app I'm able to put in different scenarios and it uses AI to model out what might happen to each stakeholder depending on the scenario. And you can start to see like the second order and like third order effects of things. So I thought that was like a fun little app to use.
Justin Venneri: (11:51) Which scenario did you start with, out of curiosity?
Andrew Tsang: (11:54) One of the things is people were talking about AI and I had built this on AI. There's a lot of momentum around AI powered prior authorizations. So I think they announced that at AHIP a couple months ago. Yeah, we're going to start doing the majority of our prior authorizations using AI. And it's funny, so I punched that in and it's kind of surprising because most people, especially Patients and consumers really don't like the idea of prior authorizations and more importantly providers really hate it.
Justin Venneri: So what would happen if they implemented an AI powered prior auth and hopefully speed things up and how that balance shift or how the seesaws tilt on that one?
Andrew Tsang: Well, I mean this is just like a projection. If I could predict the future, I would be doing a lot more.
Justin Venneri: Oh yeah, we’d be on the beach is the old saying.
Andrew Tsang: (12:35) Yeah, but as far as that goes it is surprising because you see with that actually the patients and providers don't get as big wins as the payers might. Right. Because for payers they reduce a lot of costs in reviewing prior authorizations and they have faster processing and more consistent decision making. But providers, this is a big workflow disruption for them. So if they get a bunch of AI denials they gotta handle these escalations. Right. So sure, provider orgs will have different carve outs for different delays so that they can kind of catch up operationally. But what's really surprising is that the patients, right, like yeah, this is great that you know, faster decisions will be made but there is a risk that AI then has inappropriate denials in place. So then you know, you're up arguing against a machine trying to appeal different, you know, treatments and services.
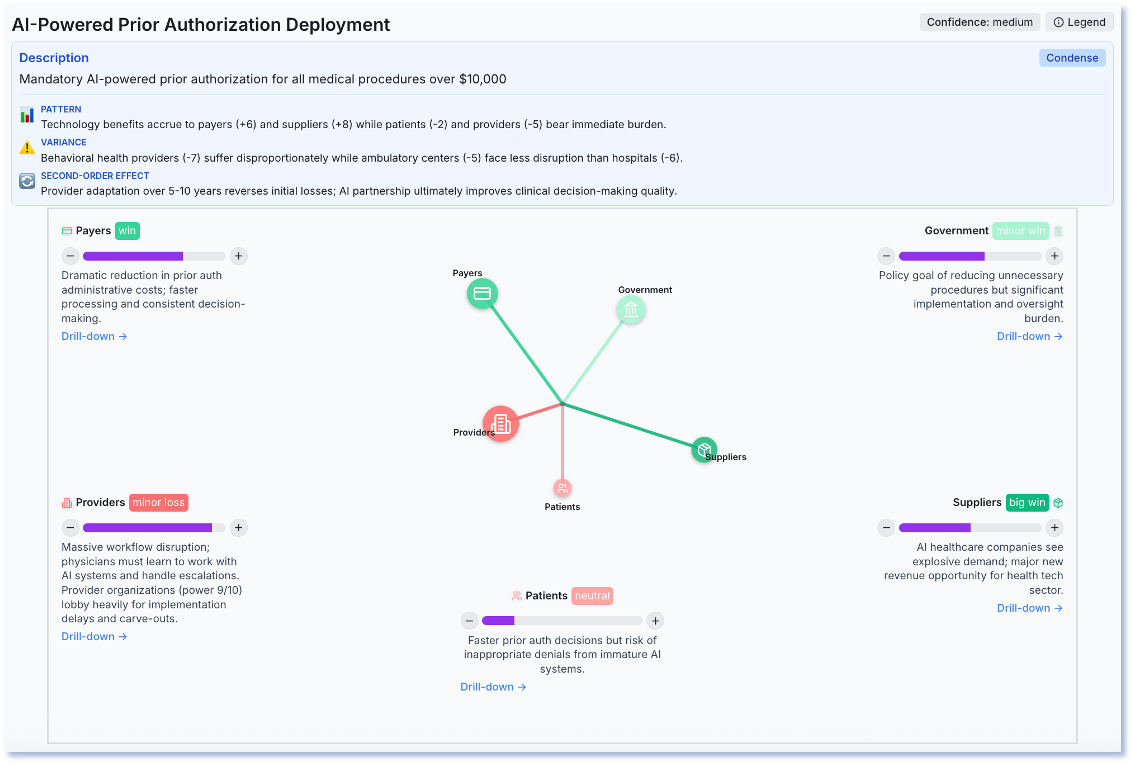
Justin Venneri: (13:23) Oh, it's fascinating. So the model is basically saying be careful what you wish for.
Andrew Tsang: (13:27) Oh yeah. I mean that's the thing about healthcare, we've got a lot of great intentions on how to do it. It's really hard to think about the practical trade offs.
Justin Venneri: (13:34) Got it. I think I saw another one. It was a “Big Tech Healthcare Platform Entry” [scenario] and the disruption that would cause winners and losers. How'd that one shake out?
Andrew Tsang: (13:42) Yeah, I mean realistically we haven't seen that yet. Like we've seen Amazon try to enter Healthcare, Apple, right. Maybe CVS. If they build like a big primary care outpatient system it'd be surprising to see who would benefit or lose on this. Well for one traditional practices would lose a lot of market share. So probably a big revenue decline there from independent physician groups or you know, even major health systems. Because big tech has a lot of scale that some other places just can't compete with payers too. They lose to some of the new players for sure because their networks are now degraded and they might not necessarily be able to reap the benefits of the new efficiencies from like these major players.
Justin Venneri: (14:24) Very cool. Well we'll put the link to this new healthcare 5-way seesaw in the show notes and people can play with that. So Andrew thank you so much for spending your time with us today, sharing your insights. Last question for you and I ask everybody, given our discussion today, I'm sure you've seen a lot, given your work and experience across the industry and the content you're producing and people you're talking to, what's the most astonishing, interesting or surprising thing that you've found? And obviously keep your compliance hat on. Please tell us a good safe to share story to send us off here.
Andrew Tsang: (14:52) I think what has been really fascinating to me is how hospitals work because I've been spending most of my time there in my career. But some people don't really fully appreciate is what loses money in a hospital. Right. And that was something that resonated when I posted it online. A lot of clinicians and executives were like, thank you for articulating this. Because you don't realize that the stuff that's core to a hospital, like saving people's lives, is the one thing that actually loses money.
Andrew Tsang: (15:17) So you know, respiratory care and pulmonology, sepsis treatment in critical care. Right. In ICUs, these things that literally keep people alive are often the services that lose money for hospitals. And you know, for the most part, people know that cross subsidization exists. You know, high margin things pay for lower margin things. We see this in other economies as well, right. Costco doesn't make money on hot dogs and chickens. They, you know, make money on memberships. But in healthcare, it's a lot harder when your loss leaders are, you know, based on saving someone's life. So if we're trying to make things more cost efficient in healthcare, you have to come to a real decision that keeping an ICU open and knowing that it loses money makes it really difficult to make business decisions on it. So I think we have to come to a reckoning. And I thought that was something that was really interesting to me and a lot of people have shared expressing something, one of the core tensions that we have in trying to make a healthcare a better place.
Justin Venneri: (16:07) Yeah, that is a really interesting thing to keep in mind about the hospital setting. So Andrew, before we go, how can people get in touch with you if they'd like to learn more? I know we will link your Substack and everything. Would you prefer LinkedIn or some other way to reach out, subscribe, et cetera?
Andrew Tsang: (16:21) Yeah, thank you so much for sharing that.
People can find me on LinkedIn – Andrew Tsang/1219 - and then I've also set up my domain now so you can reach me @AndrewTsang – Health Is Other People on Substack there where I'll try to produce some more of my writing.
Justin Venneri: (16:35) Awesome. Well, I hope you have a great rest of your day and I look forward to staying in touch.
Andrew Tsang: (16:38) Thanks so much Justin. It was great being here.
Want to stay apprised of the latest Judi Health news? Sign up for our monthly newsletter!
Interested in transitioning to an aligned and transparent pharmacy and health benefit partner? Click here to get in touch with our team!
Disclaimer
This podcast is for informational and entertainment purposes only. The views expressed are those of our guests, do not constitute professional advice, and may not represent Judi Health's/Capital Rx's position on any matters discussed. We make no representations or warranties regarding the accuracy or completeness of the content; information is subject to change and may not be updated.


.jpg)







