
Transparent pharmacy benefit management, perfected
There's a new standard for pharmacy benefits. With clear fee-based pricing, a next-generation enterprise health platform, including AI-enhanced workflows, and no conflicts of interest, we’ve realigned the stars to deliver a pharmacy benefits experience that exceeds plan sponsors’ and plan members’ needs.
Cost Savings
Transparent pricing means clear, predictable costs
With a Single-Ledger Model™, understanding what the plan and its members pay for their medications is simple. There’s no spread, no hidden fees, and 100% pass-through of pharmaceutical manufacturer revenue.
Transparent pricing
Enjoy full budgetary control with our clear, no-hidden-costs pricing model.
Advanced technology
Advanced technology for faster program administration and superior results.
Partnership & collaboration
We don’t just provide services; we collaborate with you – because your success is our success.
Clinical programs & prior authorization
Through our robust programs, we provide optimal health expenditure and improved patient outcomes.
Exceptional service
Our superior customer service means fewer calls and more time to focus on your core business.
Customized solutions
We tailor our pharmacy benefits to meet your unique needs, offering a perfect fit for every client.
.png)
When it comes to manufacturer revenue, details matter
Understanding what a health plan and its members pay for medications is simple when there's 100% pass-through of pharmaceutical manufacturer revenue and no spread pricing or hidden fees.
.jpg)
100% pass-through to clients, with minimum guarantees
Rebate definition includes all manufacturer revenue streams
NDC-9 reporting allows full visibility into drug-level economics
Manufacturer contracts auditable via dynamic virtual review process
Aggregator retention is tiered based on BOB growth
Drug prices are freely available
Capital Rx's preferred price benchmark, National Average Drug Acquisition Cost (NADAC), has several advantages over other drug price benchmarks. So, we created a national network that improves transparency, equity, and access to medication.
%20(1).png)
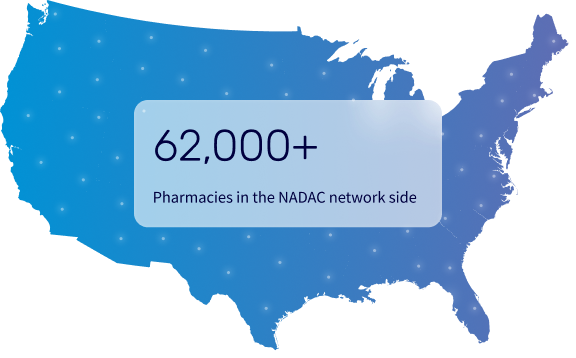
NADAC provides a rational alternative to AWP & MAC lists
With NADAC:
All plan members receive the same prices across a network of 62K+ pharmacies
Plan fiduciaries can see the prices paid for drugs
Plans benefit from drug price deflation
Retail pharmacies are reimbursed in a transparent manner
Fiduciary Alignment
Trust is everything, especially when it comes to compliance. Capital Rx’s aligned business model and transparent pricing carry no hidden costs or conflicts of interest.
We believe in uniform pricing and provide complete access to claims data, rebate payments, and network reimbursement, all while helping plan sponsors stay compliant with ERISA fiduciary requirements.

“Capital Rx continues to make strides in amazing me with its capabilities. They ride the crest of the wave in the PBM market. I couldn't ask for a better team to oversee my members. They will always do anything in their power to accommodate your needs. They are a PBM that other PBMs need to look out for because they are staying at the forefront!”
Maria Scheeler, Executive Director, Administrator
Teamsters Health & Welfare Fund of Philadelphia & Vicinity
customer care
Putting plan members first, always
Expertise matters in customer care, especially for pharmacy benefits. Arming Pharmacy Technician Certification Board (PTCB) certified pharmacy technicians and other healthcare professionals with modern, AI-powered technology yields incredible results.
Modern tech
Leveraging the future of pharmacy benefit administration technology, today
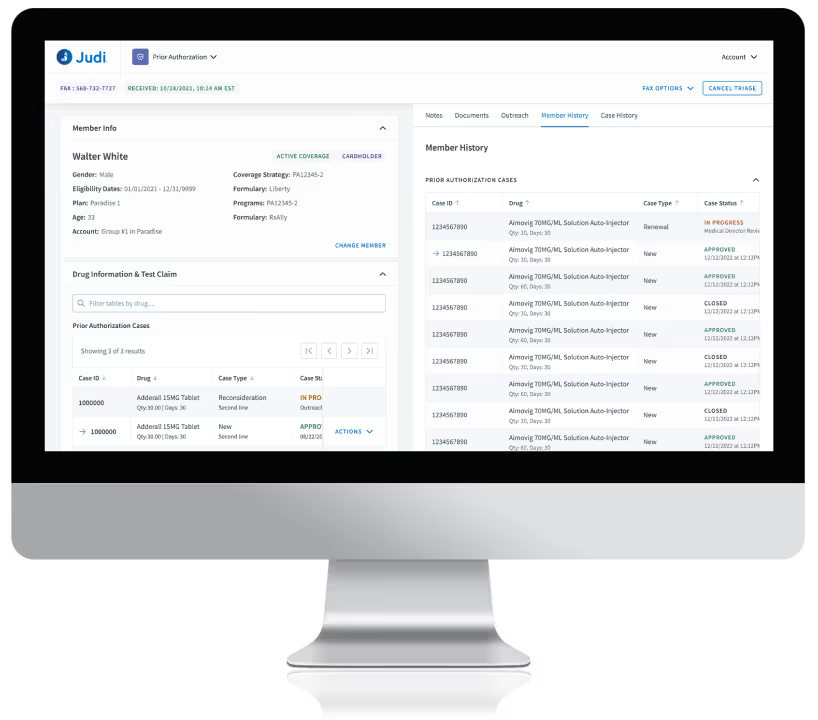
Capital Rx efficiently serves clients ranging from hundreds of lives to hundreds of thousands of lives, thanks to its proprietary enterprise health platform: Judi®.
Every workflow and process in one intuitively designed system
Data available on demand
Connect to or integrate with any other vendor
Make rapid changes via patented technology
Clinical programs powered by modern technology
Utilization management
Ensure appropriate prescription coverage
Cost containment
Lower prescription spend
Patient safety
Prevent adverse drug events
Population health
Improve performance of quality measures (Stars, HEDIS, etc.)
High-touch personalized care
Optimize medication therapy outcomes
.png)
.png)
Member service
A member app designed for ease of use and real-time access to information
Clean and user-friendly design and interface. It offers comprehensive functionality for member access to all key aspects of the pharmacy benefit:
Find a prescription at a nearby pharmacy
See real-time prior authorization status updates
View deductible levels
Available for iOS & Android
FAQ
Frequently asked questions
What is a pharmacy benefit manager?
A Pharmacy Benefit Manager (PBM) is an administrator who processes prescription drug claims on behalf of payers, such as employers and health plans.
The role of a PBM also includes handling numerous other behind-the-scenes processes, from plan design to real-time data exchange, payments, eligibility, card printing, formulary management, and much more.
Is Capital Rx a transparent PBM?
Yes! Capital Rx is a transparent PBM in all aspects of pharmacy benefits management. We never earn revenue on drug spend, pass through 100% of manufacturer rebates to employers, and leverage a public pricing benchmark – National Average Drug Acquisition Cost (NADAC) - to offer trustworthy and reliable visibility into drug pricing.
What is NADAC and why does Capital Rx use it?
NADAC is a public benchmark calculated by the Centers for Medicare and Medicaid Services (CMS) that reflects the average amount pharmacies pay wholesalers for medications. As opposed to Average Wholesale Price (AWP), which is based on wholesale pricing data that private companies collect from drug manufacturers, and does not include rebates or discounts, NADAC offers a fair and transparent view into real drug costs. Capital Rx uses NADAC to provide fair and transparent pricing for clients and transparent reimbursement to pharmacies. Additionally, NADAC’s public availability allows clients to hold us accountable for our transparency as a PBM.
How does implementation work with Capital Rx?
Capital Rx delivers a seamless and efficient implementation experience. Our dedicated team guides clients through every step, facilitating smooth data migration and integration with existing systems, minimizing member disruption by addressing concerns promptly, enabling continuity of care, and helping maintain existing pharmacy relationships where possible.
How does Capital Rx handle rebates from drug manufacturers?
Capital Rx passes 100% of drug manufacturer rebates through to clients, eliminating hidden fees and redirecting all financial benefits to them.







.png)
.png)
.png)
.png)
.png)
%20(1).png)
.png)
.png)
.png)

%20(1).png)
.png)

