Health Benefits 101: Service Excellence & Scaling an Award-Winning Call Center Model

Customer care is unique in healthcare because it’s one aspect of the system that almost everyone touches. When a call comes through our customer care center, that’s the moment when a system designed on paper meets a real person who needs answers, often quickly. A question about a claim, confusion about drug coverage, or perhaps there's an access issue – these are personal problems. As a result, the call center becomes the core of where trust is earned.
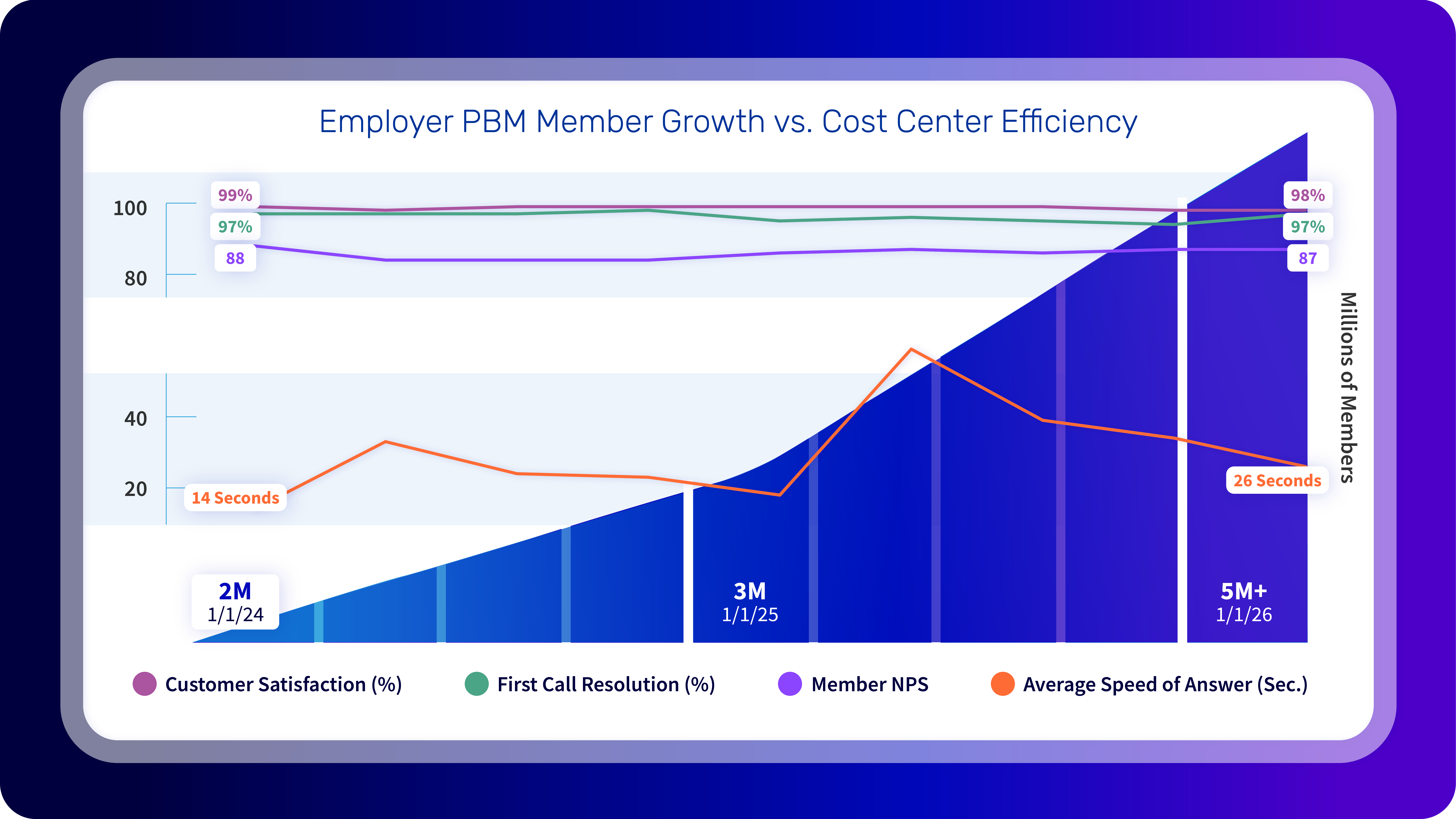
At Judi Health, our goal is to help people - our clients and their plan members - understand what is happening, what their options are, and what comes next without rigid scripts or being shuffled between teams or left guessing. This approach has led us to recognition and consistently strong satisfaction outcomes, proven by our member NPS (Net Promoter Score) of 87 and a 98% customer satisfaction rate. More importantly, our approach has shaped a service model grounded in accountability and care.
Will Tafoya, Senior Vice President of Customer Care, helped design this model from the ground up, with this approach earning the team a Gold Stevie Award for Achievement in Customer Experience and a CCW Award for Customer Contact Leader of the Year in 2024. His perspective is simple and direct: “One of the things I’ve learned over the years is that customer care has to be knowledgeable about everything that occurs within the organization to be able to effectively serve the plan sponsor or member that’s calling.” That belief is foundational here; if the frontline doesn’t have the context, tools, or authority to solve problems, service becomes a loop of transfers and apologies. So, we built something better.
Increasingly and simultaneously, the market is demanding better. In episode 84 of our Astonishing Healthcare Podcast on how the PBM RFP process is evolving, Josh Golden, SVP of Strategy and Nic Bolitho, Manager of RFP Content, described a clear shift: the old, spreadsheet-first evaluation model is ineffective and narrowly focused. Plan sponsors are asking sharper questions, expecting real accountability, and looking harder at what actually happens when members need help. This is exactly where an award-winning customer care organization becomes more than a “nice-to-have.” It becomes a differentiator.
Why Customer Care Matters More Than Ever in Pharmacy Benefits
Members typically aren’t calling to understand contract language or rebate mechanics. They’re calling because something doesn’t make sense; it feels wrong, or it’s standing between them and their medication.
Though member calls tend to follow similar patterns, they rarely feel routine to the person making them. A rejected claim raises immediate concern about cost. A prior authorization delay can feel like a barrier to care. A pharmacy transition can leave someone unsure of what to do next. These are high-stress moments, and how they are handled shapes trust in the entire benefit, not just the call center.
Plus, as pharmacy benefits have grown more complex; the nature of calls has become more sensitive. Specialty drugs, GLP-1 therapies, tighter utilization management, and more frequent plan changes have caused members to encounter more roadblocks than they did even a few years ago. When those moments happen, customer care becomes the defining touchpoint of the experience.
Sonia Pettis, Manager of Customer Care Operations, and Lisa Ellerhorst, Senior Director of Customer Care Operations, joined us in episode 86 of our Astonishing Healthcare Podcast to discuss their insights and approach to our customer care operations.
“Some of our top call drivers include claim status, mail order, drug coverage, and eligibility,” said Sonia, also pointing to one of the most common pressure points: “We encounter members that call to ask about GLP-1 medication coverage – our members want to know why the claim was rejected and what steps can be taken to resolve the issue.”
What defines the experience is how the call is handled. When a claim is rejected, members need an explanation that makes sense without jargon. When a prior authorization is required, they need guidance and support, not another hurdle. When prescriptions move between fulfillment channels, members shouldn’t have to manage the handoffs themselves.
This is where our model shines. Sonia described how the team responds after identifying a rejection: “Once our team identifies the issue, we always make sure to clearly explain the reason for the rejection to our member. If a prior authorization is necessary, we’ve offered to reach out to their prescribing physician to start the process, ensuring that our members have a smooth and supportive experience.”
This is what a real member-first approach looks like.
Experience Makes Resolution Possible, and Resolution Beats Speed
In healthcare, rushing an interaction often leads to incomplete explanations and repeat calls. That can make a member feel stuck. That is why our customer care model is built around resolution, not arbitrary handle-time targets, and most definitely not a ‘get them off the phone and hope it works out’ approach.
Echoing Will’s explanation of why we don’t measure average handle time – or have an average handle time target for calls, Sonia simply stated: “We do not measure success by speed. We’d rather focus on thoroughness, carefully reviewing benefit details and engaging our clinical team when appropriate.”
This is a practical strategy. Members call because they need clarity and next steps, and thoroughness reduces repeat contacts, lowers confusion and frustration, and builds trust.
However, resolution at this level requires experience that helps us maintain our 97% first call resolution rate. Customer care in pharmacy benefits is not an entry-level function, requiring working understanding of how benefits are administered, the process of how claims adjudicate, where, or how, prior authorizations get stuck, and how clinical decisions intersect with coverage and cost. That is why Judi Health has invested in experienced talent, including Pharmacy Technician Certification Board (PTCB) certified professionals and team members.
Lisa Ellerhorst has seen firsthand how experience and scale support quality. A “well scaled operation reduces burnout, improves our training outcomes, and creates a more supportive environment for our frontline teams, [leading] to better performance and lower attrition.”
When volume increases and complexity rise, that foundation matters. Even while managing significant growth, our team has maintained exceptionally high satisfaction because expertise is built into the model.
Collaboration, Alignment, and Technology are now RFP-Level Requirements
Great customer care doesn’t operate in isolation, and increasingly, plan sponsors are unwilling to accept service models that do. In pharmacy benefits, the call center sits at the intersection of clinical teams, operations, finance, vendor partners, and clients. When those groups are aligned, service is seamless. When they’re not, even the smallest issues can escalate quickly.
This is showing up in the procurement process. Josh described “tectonic shifts” in the market, and was blunt about what’s changing: employers are moving away from “unit cost” spreadsheets and toward a broader evaluation of PBM behavior and accountability, including the experience members have interacting with us every day.
He also called out the problem with traditional members experience questions. “Back in the early days, employers were asking open-ended questions, and frankly, that’s just an invitation for a lot of marketing fluff.” Instead, he said plan sponsors are now asking “more precise and specific questions that get at the things that matter,” including “What is your net promoter score?” and “What’s your average turnaround time for moving a prior authorization through your system?”
What plan sponsors are ultimately looking for in these RFPs is proof of operational truth and evidence of how customer care actually functions. PBMs have to demonstrate how their service model performs under real conditions, whether volume increases, benefits change, or members encounter friction:
Judi Health’s customer care model was built to withstand that level of scrutiny, which ultimately comes back to management. After all, the most important letter in PBM is the “M.” Josh always stresses that how a PBM manages utilization, workflows, and member interactions once a plan is live matters far more than how the model looks in a spreadsheet.
Customer care is where that management comes visible, and technology is what makes it possible at scale. Without real-time access to accurate information, even well-trained teams are limited in what they can resolve during a single interaction. Modern platforms are necessary infrastructure that allows service team members to deliver clarity while maintaining accountability and consistency, and for us, that foundation is Judi®.
What Award-Winning Service Actually Feels Like
Even as call volume has grown, Judi Health’s care team has maintained high satisfaction by staying focused on resolution and empathy. Beyond formal metrics, some of the most meaningful feedback comes from unsolicited recognition, moments when members reach out simply to express their gratitude for the support they received. Lisa Ellerhorst described these “kudos” as powerful reminders on the impact thoughtful service has on real people.
Building our call center in pharmacy benefits is about designing services around people, investing in experience, and holding the line on quality as complexity grows. Customer care is where pharmacy benefits become real and treating it as a strategic priority is not optional. That’s who we are.
Want to see how good our customer care team is? Don't take our word for it. If you're a member, give them a call any time, 24/7/365, and see how quickly you can talk with one of our representatives.


.jpg)


-p-2000.jpg)




